Following on from last week’s post regarding the BNF’s (British Nutrition Foundation) briefing paper (Hart, KH et al 2025), this week I will be covering the advice given to pregnant women.
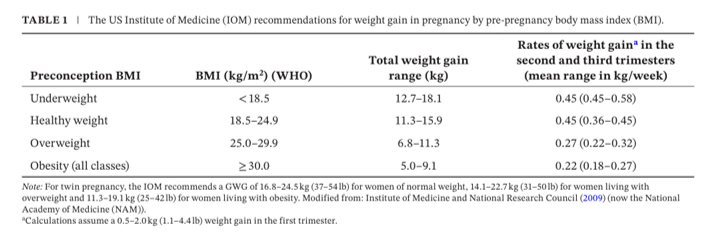
Currently there are no evidence-based guidelines for weight gain during pregnancy and no routine weighing takes place unless there is a clinical need. A mother can request her weight be monitored and NICE guidelines suggest in those cases to use the US Institute of Medicine guidelines to estimate healthy weight changes based on pre-pregnancy BMI, these are shown below.
Overweight/obesity can influence rises in blood glucose levels that can lead to gestational diabetes, a common impact of pregnancy as a result of an increase in insulin resistance so that glucose can be redirected to the growing fetus. Problems arise when the insulin secretion does not adequately match the degree of insulin resistance leading to maternal blood glucose rises and increased risk of higher birth weight, stillbirth, early delivery and development of type II diabetes for mother later in life.
During pregnancy metabolic changes take place that result in a more efficient uptake and absorption of nutrients which is why no extra increase in dietary intake is required if following a diet based on the UK recommended Eatwell Guide (PHE, 2016). Some increase in nutrients are recommended at certain points during pregnancy, a summary is shown below.

Energy needs do not change until the last trimester when an increase is recommended of 200kcal/day.

Protein is essential for fetal growth and cellular development as well as maternal metabolism changes and tissue development. The UK recommends an additional 6g/day increased intake; this has been calculated on a woman of average weight of 60Kg so requirements can vary but it is not recommended to exceed intake more than twice this amount. Animal proteins are the preferred source as they contain all of the essential amino acids required, this can also be obtained through plant-based proteins just ensure a varied amount are eaten throughout the day.
Vitamin A, thiamine, riboflavin, folate and vitamin C should all be increased slightly to support fetal growth and energy metabolism, care should be taken not to exceed 1500ug/day of vitamin A as this can result in very serious teratogenic effects.
Calcium and iron inadequacies in pregnancy are common so although on extra intake is required, care should be taken to ensure adequate dietary consumption. Increased blood volume and fetal requirements can lead to low iron, rich dietary sources are beef, offal and fish, leafy greens and dried fruit. Calcium is important for bone and teeth development of the baby and inadequate supplies can lead to demineralisation and weakened bones of the mother.
Adequate hydration is essential, at least 1.6L/day is UK recommended, fluids should be consumed throughout the day, water and milk are good choices. Caffeine should be kept to a minimum, no more than 200mg/day, too much can lead to spontaneous abortion and low birth weight.
There is no safe level of alcohol intake during pregnancy, it can lead to myriad negative impacts that vary from premature birth to learning and behavioural disorders of the baby, avoid at all costs.
References
Hart, K. H., Hill, A. J., Gonzalez, J. T., de la Hunty, A., Gallagher, A. M., & Stanner, S. A. (2025). Diet in Pregnancy: A Review of Current Challenges and Recommendations. A British Nutrition Foundation Briefing Paper. Nutrition Bulletin.
PHE. (2016). The Eatwell Guide. London, Public Health England