The BNF (British Nutrition Foundation) published an important briefing paper last month (Hart, KH et al 2025) as an update on guidance relating to nutritional advice for women during pregnancy in the UK, they reviewed relevant data relating to current challenges and gave recommendations. In order to cover this extensive material, I am splitting it over two posts, this week pre-pregnancy.
The first 1000 days of a child’s life; the period from conception to 2nd birthday, are considered to be a crucial period with regards to adequate nutrition, Barker et al first proposed the concept of the fetal origins of disease back in 1989, they highlighted the link between low birth weight and increased risk of cardiovascular disease, type II diabetes and other metabolic syndromes. Numerous longitudinal follow-up studies have since backed up this hypothesis that both under and over-nutrition within this early period correlate with an increased risk of chronic disease later in life for the child.
Pre-pregnancy dietary advice recommends women adhere to general healthy eating principles outlined within the Eatwell Guide (PHE, 2016) with special attention to the following nutrients:
Vitamin D – Essential for healthy immune function and bone development, it is recommended that all of the population including those women planning to get pregnant supplement 10ug/day from March to October.
Folate/Folic acid – Essential to avoid the formation of fetal neural tube defects. The recent NDNS survery highlighted low levels within women of childbearing age, supplementation of 400ug/day is recommended pre-conception until the 12th week of pregnancy.
Iodine – Important for fetal brain development, the recent NDNS also showed levels within women and young girls, it is currently recommended that this is obtained through diet (see below), those that choose to supplement are recommended to take a maximum of 150ug/day in the form of potassium iodide/iodate, NOT those sourced from seaweed.
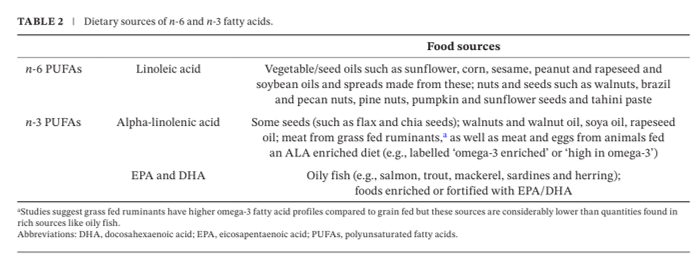
Essential Fatty Acids – Linoleic acid (LA), alpha-linolenic acid (ALA) and their longer chain derivatives EPA and DHA are all essential to new tissue formation so important to take pre and during pregnancy to support fetal development. EPA and DHA are primarily sourced from oily fish and other dietary sources are outlined below. Supplementation has been shown within randomised controlled trials to suggest some benefits including extending gestation, increase birth weight and a potential reduction in preterm births and perinatal death risk. Public health guidelines suggest supplementing DHA at 100-200mg/day, make sure the supplement does not contain additional high vitamin A content for e.g cod liver oil.

Fertility in women is affected by their % body fat rather than absolute body weight. Women who maintain a low % body fat can suffer from irregular menstruation which can lead to longer time to conceive and more likely to conceive. Excessive fat stores can impair fertility by an estimated 3% for every increase above a healthy BMI of 19.5kg/m2.
Obesity can impact all stages of conception, this is thought to be due to the impact on hormone profiles as well as other factors. It is recommended that weight loss or gain to attain a BMI of 18.5-24.9 Kg/m2 to increase chance of conception and maintaining a healthy weight through pregnancy, this is important as evidence shows that excessive weight gain during pregnancy is associated with increased risk of gestational diabetes, hypertensive disorders, pre-term birth and a long term risk of obesity for both mother and child.
References
Hart, K. H., Hill, A. J., Gonzalez, J. T., de la Hunty, A., Gallagher, A. M., & Stanner, S. A. (2025). Diet in Pregnancy: A Review of Current Challenges and Recommendations. A British Nutrition Foundation Briefing Paper. Nutrition Bulletin.
PHE. (2016). The Eatwell Guide. London, Public Health England